Centene Vision Services is a leader in exceptional, tailored vision benefits and services for Medicaid, Medicare, and Marketplace member products. Every quarter we share key news that you can use to best serve your patients.
More States to Offer Ambetter Solutions, an Alternative to Group Insurance
 Centene Vision continues to grow in the Ambetter Health marketplace. For 2026, we are adding Ambetter Solutions ICHRA* plans across the country, bringing the total to 13 states in which ICHRA plans are available: Arizona, Florida, Georgia, Indiana, Kansas, Missouri, Mississippi,.Nebraska, Ohio, Oklahoma, South Carolina, Tennessee and Texas
Centene Vision continues to grow in the Ambetter Health marketplace. For 2026, we are adding Ambetter Solutions ICHRA* plans across the country, bringing the total to 13 states in which ICHRA plans are available: Arizona, Florida, Georgia, Indiana, Kansas, Missouri, Mississippi,.Nebraska, Ohio, Oklahoma, South Carolina, Tennessee and Texas
Currently just 56% of small businesses in the U.S. offer health insurance. ICHRAs are a new approach to employer-sponsored health benefits. With options that are affordable and require less hands-on administration, ICHRAs can help more employers provide health and vision insurance coverage. From 2023 to 2024, the number of companies offering an ICHRA grew by nearly 30%.
Rather than being assigned a group insurance plan, each employee chooses their own insurance on the health insurance marketplace, subsidized by a pre-tax employer contribution. Employees also can maintain their healthcare coverage even if they leave the company.
These flexible insurance options are especially appealing for employers that:
- Have a diverse workforce with different healthcare needs
- Employ workers in multiple states without a single-carrier solution
- Want to offer health benefits/more choice to attract talent
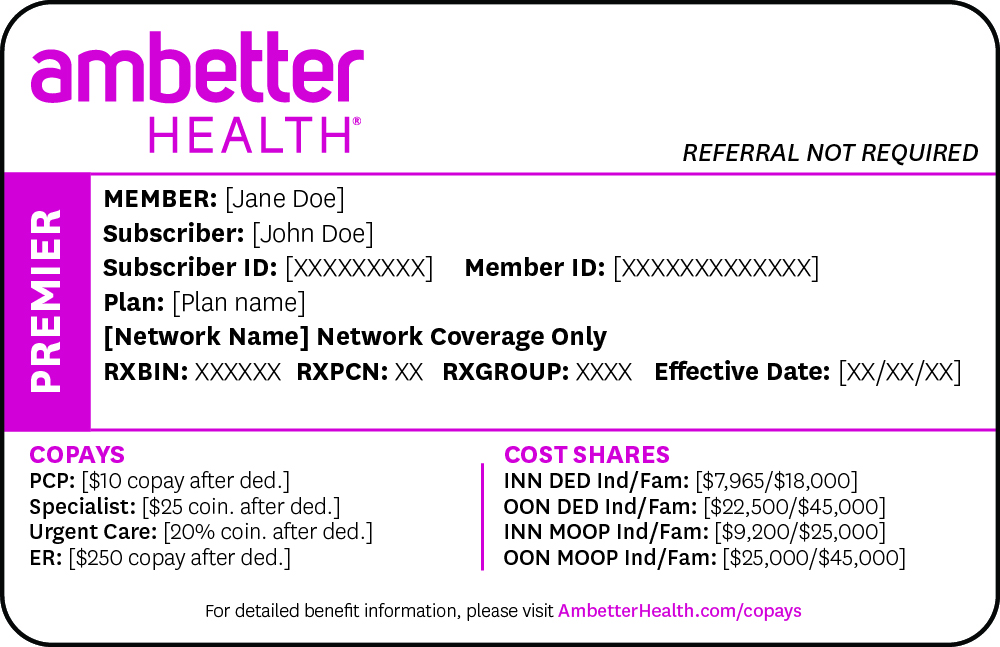
In addition to bringing new patients to your practice, Ambetter Solutions plans are easy to understand because they offer the same Ambetter vision benefits you already know. Simply confirm the member’s Ambetter Solutions ID card and eligibility by logging in to our provider portal. Please refer to our most recent Ambetter Health Plan Specific for more details.
Better coverage and perks have made Ambetter Health America’s number one marketplace health insurance. And now, ICHRAs mean we can offer coverage to even more people than ever before. Thank you for being a valued part of our vision network!
*Individual Coverage Health Reimbursement Arrangement
Wellcare Medicare Adds Vision Coverage and New Dual Plans in Two States
 As we approach 2026, Wellcare Medicare Advantage is introducing some exciting updates. Centene Vision will now offer vision benefits in two additional states: Ohio and South Carolina.
As we approach 2026, Wellcare Medicare Advantage is introducing some exciting updates. Centene Vision will now offer vision benefits in two additional states: Ohio and South Carolina.
We are reintroducing standard Medicare Advantage vision benefit coverage, but we’re also introducing Dual Aligned plans.
- Wellcare Medicare Advantage plans provide vision coverage under the Wellcare Medicare brand in Ohio and South Carolina.
- NEW! Wellcare Dual Align plans combine Wellcare Medicare Advantage and state Medicaid vision benefits. To ensure payment for all covered vision services, providers serving these members must be contracted with Centene Vision for both Medicare Advantage and Medicaid. Dual Aligned plans will be available in Ohio and South Carolina.
Providers should always verify eligibility before rendering services. For individual member benefits and eligibility, access our Eye Health ManagerExternal Link (EHM). You may also call Customer Service to reach our automated member eligibility-verification system or a team member.
Wellcare Spendables™: The Wellcare Spendables Card is being offered again in 2026 with a change in administrator. Members will now receive a preloaded CareCredit card that can be used to cover eligible out-of-pocket vision expenses in offices that accept CareCredit. All transactions with the Wellcare Spendables card will need to be processed through CareCredit’s provider portal, called Provider Center. For more information visitExternal Link carecredit.com/providers.
Check the EHM for 2026 Provider Manual and Plan Spec Updates
As a reminder, annual updates are made to the Vision Provider Manual, so always check the EHMExternal Link at centenevision.com/logon for the most updated version. Please refer to the manual, along with the custom Plan Specific for your particular state and product, before providing services to members.
Local Market Reminders
Below are important upcoming changes:
- Arkansas Medicaid – Beginning January 1, 2026, Medicaid vision benefits will be administered by the state. Centene Vision will no longer be administering benefits for Arkansas Total Care, but all claims with a date of service of 2025 will be processed by us.
- California Medicaid – Health Net will transition their commercial plan for routine vision services to EyeMed effective January 1, 2026.
California Health Net provider must complete the annual provider training by December 31, 2025.* - Illinois Ambetter – Effective January 1, 2026, Centene Vision is transitioning the management and claims adjudication of medical eye care services delivered by ophthalmologists for all Illinois Ambetter Health members to Meridian Health Plan. Ophthalmologists on the Centene Vision panel must file medical and surgical vision claims with Meridian Health Plan instead of Centene Vision. There is no action needed on your provider contract in advance of this transition.
- Medicare-Medicaid Plan (MMP) Terminations – In 2026, MMP plans in Ohio and South Carolina are being transitioned to Dual Aligned plans.
- Nevada Medicaid – SilverSummit Health Plan will expand its Medicaid managed care service area to include all NV counties effective January 1, 2026.
- Wellcare of North Carolina Marketplace – WellCare of North Carolina will discontinue the Marketplace product December 31, 2025.
- Pennsylvania CHIP – Beginning January 1, 2026, Centene Vision will be administering vision benefits for PA Health and Wellness CHIP members.
- Texas Medicare Advantage – Beginning January 1, 2026, El Paso Health is adding two new Medicare Advantage plans, Health Total and Health Giveback.
- Texas Medicare-Medicaid – As directed by CMS, the current Superior HealthPlan STAR+PLUS Medicare-Medicaid Plan (MMP) will sunset on December 31, 2025. Members may choose to enroll in a new D-SNP Medicare plan for 2026 instead.
* Registered California Medicaid providers are required to complete Annual Compliance training. The training is due December 31, 2025. If you have completed this attestation after October 1, 2025, no action is required. Please contact ebocompliancematters@centene.com with any questions. Link to training: centenevision.com/catrain
Improve the Health of Diabetic Members
 Help your patients with diabetes and reduce administrative burdens. Centene Vision Services offers a dedicated HEDIS Training and TipsExternal Link website to determine CPT II and other supplemental codes to use for diabetic retinal exams. Routine retinal evaluation is recommended to reduce the risk of diabetes-related blindness.
Help your patients with diabetes and reduce administrative burdens. Centene Vision Services offers a dedicated HEDIS Training and TipsExternal Link website to determine CPT II and other supplemental codes to use for diabetic retinal exams. Routine retinal evaluation is recommended to reduce the risk of diabetes-related blindness.
You may be eligible for a $10 CPT II reporting incentive. Please ensure your billing staff submits a billed rate of at least $10 to receive the maximum reimbursement for this incentive program. Review your fee schedule and remember to submit the appropriate CPT II codes referenced at HEDIS Training and TipsExternal Link.
REMINDER: Glaucoma disproportionately affects Black and Hispanic individuals. They are more likely to develop vision loss and experience blindness from glaucoma than White individuals.
 Clinical Policy Updates
Clinical Policy Updates
Our clinical policies have undergone annual review, and many have been updated. Some of the changes include new ICD-10 codes for secondary angle closure glaucoma, multiple sclerosis, and thyroid orbitopathy. Below is the list of policies that have been updated. To stay up to date on all changes, be sure to use our Eye Health ManagerExternal Link provider portal or visit our policy page.
| CP.VP.05 | CP.VP.29 | CP.VP.54 | CP.VP.76 |
| CP.VP.06 | CP.VP.31 | CP.VP.61 | CP.VP.82 |
| CP.VP.12 | CP.VP.32 | CP.VP.63 | CP.VP.86 |
| CP.VP.14 | CP.VP.35 | CP.VP.64 | CP.VP.88 |
| CP.VP.16 | CP.VP.37 | CP.VP.67 | CPG.VP.22 |
| CP.VP.21 | CP.VP.40 | CP.VP.68 | |
| CP.VP.26 | CP.VP.41 | CP.VP.70 | |
| CP.VP.28 | CP.VP.43 | CP.VP.74 |
Vision Care by the Numbers
Centene Vision Services Proudly Serves
 | 30 | STATES + PUERTO RICO |  | 26,000 PROVIDERS |
 | 760,000 MEDICARE LIVES |  | 5M | MARKETPLACE LIVES |  | 10M MEDICAID LIVES |
*Data is current as of November 2025
About Us
A subsidiary of Centene for more than 30 years, Envolve Benefit Options, doing business as Centene Vision Services, has partnered with vision care providers across the country to administer eye care programs that meet the needs of our members. You are among 26,000+ unique eye care providers, including independent providers and popular retail chains, within our network. Thank you for partnering with us to provide quality vision services to your patients.

